Benign Prostatic Hyperplasia
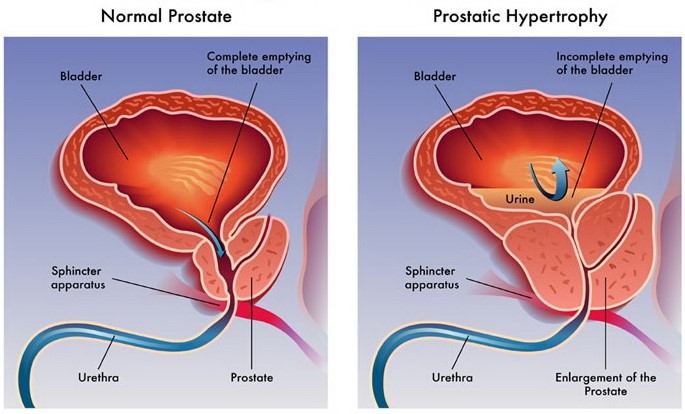
Benign prostatic hyperplasia (BPH) is a benign (non-cancerous) condition that develops when the prostate gland enlarges. As the gland grows, it can squeeze the urethra, the tube in the penis connected to the bladder where urine flows through during urination, blocking the flow of urine. The bladder becomes thicker as it works to overcome this obstruction but over time it may weaken and lose the ability to urinate normally. Other symptoms include urinary frequency, urgency, frequent urination at night, dripping after urination, difficulty in starting urination.
Who is at risk for Benign Prostatic Hyperplasia?
What does the research say about Benign Prostatic Hyperplasia?
Benign Prostatic Hyperplasia (BPH) Symptoms
The symptoms of BPH are known as lower urinary tract symptoms (LUTS)
These symptoms include:
If you are experiencing signs and symptoms of BPH and are finding it difficult to perform your daily activities and maintain your way of life, contact your primary care physician immediately.
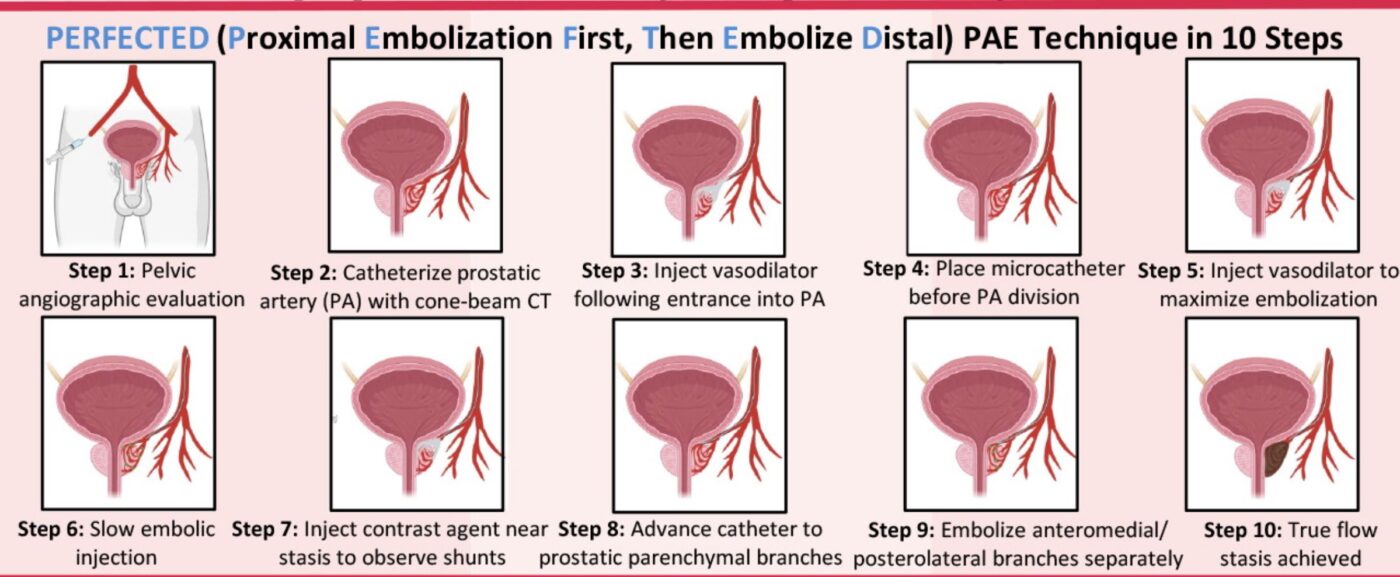
In prostate artery embolization (PAE) an Interventional Radiologist (IR) passes a catheter (small tube) through an artery in the wrist or the groin using specialized x-ray equipment. The catheter is guided into the blood vessels supplying the prostate gland. Once the catheter is appropriately positioned, embolic material (small medical particles) are injected through the catheter and into the blood vessels feeding the prostate, cutting off its major supply of blood. This shrinks the prostate over time. The embolic material remains permanently in the blood vessels in the prostate. Once embolization is complete the catheter is removed. The entire treatment typically lasts 1-2 hours and is an outpatient procedure with fast recovery times.
Non-Invasive Treatment Options
Side-effects of these treatments include sudden drop in blood pressure, abnormal ejaculation, intraoperative floppy iris syndrome (increases risks of cataract surgery), decreased libido, breast tissue development in men and more.
Surgical Treatments
Open prostatectomy
An incision is made in the lower abdomen to reach the prostate and remove the tissue. Patients with larger prostates (>80-100 cc) require open prostatectomy rather than trans-urethral resection of the prostate (TURP). Open prostatectomy is associated with a higher risk of bleeding requiring blood transfusion, erectile dysfunction, retrograde ejaculation, blood clots in the legs or pelvic veins which could occasionally cause clots traveling to the lung vessels and incontinence. Open prostatectomy requires hospitalization following the procedure.
A scope and cutting instrument is inserted into the penis and the inner part of the prostate is cut and removed. This surgery is limited to prostates <80-100 cc in volume. Up to 75% of men undergoing TURP can experience retrograde ejaculation. Other risks include urinary incontinence, erectile dysfunction, and urethral strictures.
Similar procedures where a scope is inserted into the penis. The prostate gland is cut or destroyed using microwave, radio waves or laser, depending on the procedures. Risks of these procedures include retrograde ejaculation, urinary incontinence, erectile dysfunction, and urethral strictures.
Pinellas Vascular is ready to assist you with your vascular condition or concern. Send us a message and we will get back with you quickly.